Introduction to Inomyalgia
Inomyalgia is an often misunderstood chronic pain condition that affects millions worldwide. People living with this disorder experience widespread muscle pain, fatigue, and tenderness throughout their bodies. Despite its increasing recognition, inomyalgia remains one of the least understood musculoskeletal disorders due to its complex nature and overlapping symptoms with other illnesses like fibromyalgia and chronic fatigue. For many, this invisible illness brings daily discomfort and emotional challenges that interfere with normal life.
Living with inomyalgia can be confusing. Patients struggle with persistent muscular discomfort, sleep disturbances, and cognitive dysfunction that make even simple activities feel overwhelming. The condition often gets misdiagnosed or overlooked because of its similarity to other pain amplification syndromes.
What Is Inomyalgia and How Does It Differ from Other Conditions
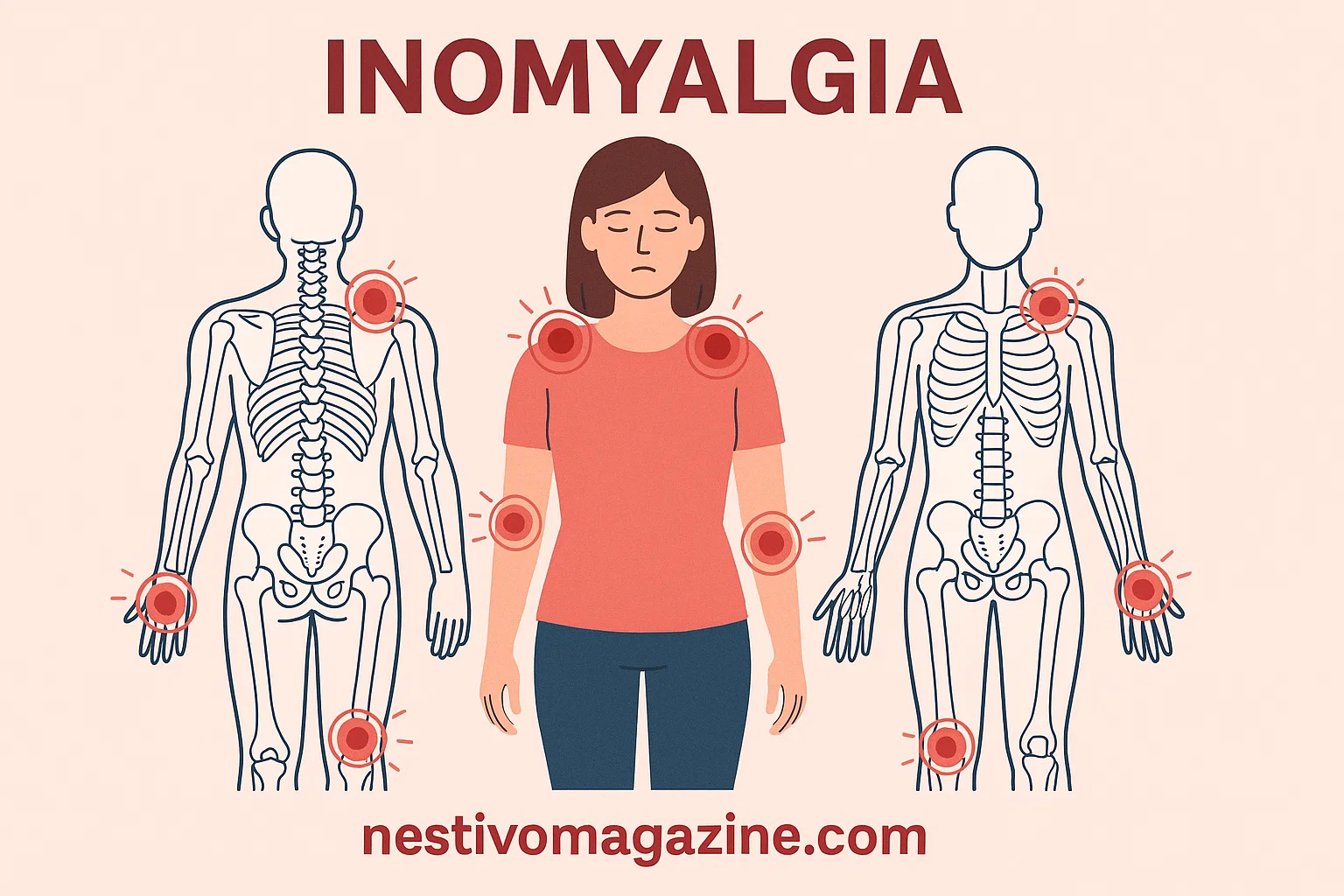
Inomyalgia is characterized by widespread muscle pain and stiffness without clear inflammatory signs. Unlike localized injuries, it affects multiple regions of the body simultaneously, sometimes involving tender points and trigger points that cause severe soreness or sensitivity.
Doctors categorize inomyalgia as part of pain amplification syndromes, conditions where the nervous system amplifies pain signals. It is closely related to fibromyalgia, but research suggests that inomyalgia may involve distinct pathways within the autonomic nervous system. These pathways regulate stress responses, and in inomyalgia, sympathetic overactivity may heighten pain sensitivity.
Symptoms and Daily Challenges
People with inomyalgia describe pain as burning, throbbing, or aching sensations affecting multiple body regions. Commonly, patients experience:
- Fatigue that seems unshakeable
- Sleep disturbances worsening fatigue and pain
- Cognitive issues making concentration difficult (often called brain fog)
- Soreness or sensitivity in multiple areas
- Emotional strain, anxiety, and frustration
These symptoms cause significant functional impairment, affecting the ability to work, socialize, or even manage daily routines. Many describe it as a hidden pain condition, where others see them as healthy but fail to grasp their struggle — the feeling that they “looks fine but feels awful.”
Causes and Triggers of Inomyalgia
Scientists have yet to pinpoint a single cause, but research suggests a multifactorial origin involving both body and mind. Some key triggers include:
| Possible Cause | Description |
|---|---|
| Genetic Predisposition | A family history of chronic pain disorders may increase risk. |
| Environmental Triggers | Exposure to cold, infections, or toxins can exacerbate symptoms. |
| Trauma (Physical or Emotional) | Stressful events or injuries often precede symptom onset. |
| Hormonal and Neurochemical Imbalance | Serotonine deficiency and nervous system dysregulation can intensify pain perception. |
The interplay between these factors leads to central sensitisation, where the nervous system becomes overly sensitive, reacting to even mild stimuli as pain.
Diagnosis: Why It’s Often Delayed
Because inomyalgia shares symptoms with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and irritable bowel syndrome (IBS), diagnosis often becomes complicated. There is no clear etiology or definitive laboratory test to confirm it. Doctors rely on medical history, physical exams, and the exclusion of other disorders.
The diagnosis often delayed adds emotional strain and isolation. Many patients visit multiple healthcare providers before receiving a proper assessment. Clear communication with a health-care provider and detailed symptom documentation can help reach a faster diagnosis.
Impact on Quality of Life
Living with inomyalgia is more than enduring pain; it affects self-esteem, productivity, and mental health. People struggle with exercise intolerance, non-restorative sleep, and emotional stress that compounds their suffering.
The combination of muscle pain syndrome and chronic fatigue reduces motivation and limits social engagement. The illness is often called a chronic invisible condition because it lacks visible signs yet deeply impacts a person’s quality of life.
Treatment and Management Approaches
Managing inomyalgia requires a multimodal treatment strategy, combining both medical and lifestyle interventions. Treatments aim to reduce pain, restore function, and enhance well-being.
Medical Interventions
- Pain medication such as NSAIDs (non-steroidal anti-inflammatory drugs) helps reduce discomfort.
- Antidepressants and antiepileptics are sometimes prescribed to balance neurotransmitters that influence pain.
- Physical therapy supports flexibility and muscle strength.
Alternative Therapies
Many find relief through acupuncture, auriculotherapy (ear acupuncture), and nutrition therapy. These methods promote circulation, calm the autonomic nervous system, and reduce muscle stiffness.
Lifestyle Changes That Make a Difference
Patients can improve symptoms through consistent lifestyle modification focusing on diet, movement, and sleep hygiene.
- Following an anti-inflammatory diet rich in fruits, vegetables, and whole grains supports recovery.
- Reducing processed sugar, saturated fats, caffeine to avoid helps manage energy and reduce inflammation.
- Supplements such as magnesium, omega-3, vitamins B/C/E, and coenzyme Q10 may assist muscle function.
Integrating mindfulness and stress reduction practices like yoga or meditation can ease physical and mental stressors as triggers.
Non-Medical Coping Mechanisms
While medical care is essential, non-medical methods enhance overall management. Regular gentle stretching and low-impact activity such as swimming or walking improves circulation and prevents stiffness.
Other effective methods include:
- Complementary medicine (yoga, tai chi, massage) for relaxation
- Balanced fluid intake for optimal hydration
- Herbal medicine / botanical support like turmeric and ashwagandha for natural relief
These form part of a holistic therapeutic approach that empowers patients to regain control over their symptoms.
Emotional and Psychological Dimensions
Chronic pain can lead to emotional strain, isolation, and misunderstanding. A supportive environment becomes vital for coping. Joining support groups and participating in patient advocacy efforts can help patients connect, share, and heal collectively.
Psychological counseling also teaches adaptability and coping strategies, guiding patients through acceptance and resilience.
A Real-World Case Study
Consider a 38-year-old woman diagnosed with inomyalgia after years of unexplained pain. Her diagnosis often delayed because initial tests showed no clear signs. Through a personalized care plan involving physical therapy, nutrition therapy, and mindfulness, she achieved gradual improvement.
Her story highlights that while inomyalgia has no clear etiology, recovery is possible through persistence, self-awareness, and medical support.
Holistic Healing and Prevention
Preventing severe flare-ups requires a holistic therapeutic approach. Maintaining sleep hygiene, engaging in low-impact activity, and following an anti-inflammatory diet can reduce the frequency of pain episodes.
A table of useful lifestyle habits for inomyalgia management:
| Healthy Habit | Benefit |
|---|---|
| Regular stretching | Enhances flexibility and reduces stiffness |
| Mindful breathing | Calms the nervous system |
| Consistent sleep routine | Minimizes sleep disturbances |
| Balanced nutrition | Supports muscle recovery |
| Staying hydrated | Prevents fatigue and muscle cramping |
The Role of Awareness and Advocacy
Raising awareness helps combat the stigma surrounding this hidden pain condition. Many patients suffer silently, feeling misunderstood. Encouraging patient empowerment and promoting educational programs can help the broader public and healthcare community understand that inomyalgia is a real and life-altering disorder.
Future Outlook and Research
Medical research continues exploring links between small-fiber nerve damage, central sensitisation, and chronic pain. Scientists aim to identify biomarkers for earlier diagnosis and better treatment. Advances in neurology and pain science may soon provide more personalized therapies and effective management options.
Conclusion: Moving Forward with Hope
Living with inomyalgia is undeniably difficult, but with the right support, management strategies, and awareness, individuals can lead fulfilling lives. By combining medical treatment, lifestyle changes, and emotional resilience, patients learn to adapt and reclaim their sense of purpose.
Though the path is challenging, embracing patient advocacy, maintaining a supportive environment, and pursuing a holistic therapeutic approach can bring strength and hope for a healthier future.
FAQs
1. Is inomyalgia the same as fibromyalgia?
No, they are related but distinct. Both cause widespread muscle pain, but inomyalgia may involve different nervous system mechanisms.
2. Can exercise worsen inomyalgia symptoms?
Overexertion can increase pain, but gentle stretching and low-impact activity are beneficial when done moderately.
3. Are there effective natural treatments for inomyalgia?
Yes, acupuncture, nutrition therapy, and herbal medicine can complement medical care and reduce symptoms.
4. How can I manage sleep disturbances linked to inomyalgia?
Follow consistent routines, avoid stimulants before bed, and create a calm sleep environment to reduce non-restorative sleep.
5. Is inomyalgia curable?
There’s no permanent cure yet, but with personalized care plans, lifestyle management, and supportive therapy, patients can experience long-term relief.